 Life is precarious – there are truly a million ways to die. And even amid tens of thousands of years of evolution, the dangers have stayed the same. Violence, accidents, natural disasters, starvation – there are many ways for man to meet his end. One hazard that has evolved alongside humans is the pathogenic microorganism – the bug (germ). These micro-toxic invaders seek entry into our bodies, to take over our physiological systems for their gain, essentially the propagation of their colonies (species) through the use of our cellular resources.
Life is precarious – there are truly a million ways to die. And even amid tens of thousands of years of evolution, the dangers have stayed the same. Violence, accidents, natural disasters, starvation – there are many ways for man to meet his end. One hazard that has evolved alongside humans is the pathogenic microorganism – the bug (germ). These micro-toxic invaders seek entry into our bodies, to take over our physiological systems for their gain, essentially the propagation of their colonies (species) through the use of our cellular resources.
But we are not sitting ducks. On the contrary, evolution has led to the development of the most efficient cellular fighting force the world has ever seen. The military might of this army executes day-in-and-day-out its prowess in keeping the human body safe and sound, despite the constant exposure to hostile invaders. This cellular soldiery is the human immune system, and it has a vast and varied genetic code that allows it to stay on top of all innovations in the pathogenic arsenal.
The immune system is complex and magnificent, and I wish to share its grand design with you here. In this article, I will explain the basics of immune system physiology, describe innate and adaptive immunity, and a few of the cells and immune factors that act as soldiers and weaponry of this legion. This article will also serve as a reference point for all future writings on immune function and how you can enhance yours. With that, I bring you the glorious human immune system.
Immune System Function
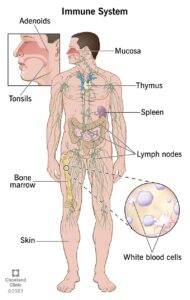
The immune system has the primary function of keeping the body free from invaders. These can include things like bacteria, viruses, and even cancer cells. Of course, it is impossible to keep invaders out completely, so when they do penetrate the body’s primary defenses, the immune system has cells that patrol the body and destroy any invading cells it encounters. Finally, the immune system keeps track of all invaders it comes into contact with. It creates an identification record so that if those pathogens are reencountered, the immune response kicks in to mobilize an active army to seek and destroy the intruders.
I particularly like to think of human immune function in terms of human military action – a metaphor that illustrates both basic and complex immunity effectively. By addressing the immune system and its function in this way, I believe it is easier to understand both its mechanism and rationale. With this analogy in mind, I think it is useful to think of the body as a kingdom, or homeland nation, or even an intricate fort. Essentially, it helps to view the body as something worth protecting, and therefore for the pathogen, also worth invading. Typically, pathogens seek entry to establish themselves in an environment conducive to their growth and propagation. What is good for them is generally not good for us, however, and so it is of utmost importance for the immune system, like a nation’s military, to be working at its highest potential.
Innate Immunity
 Innate immunity is the non-specific immune system, which we can think of as our first line of defense. It includes our fortress walls, moats, and garrison soldiers. These are the barriers and forces that keep invaders out. It is non-specific in the sense that it will work hard to keep out anything that looks foreign, regardless of type. It does not concern itself with whether it has seen the invader before or not – it is a keep-out-at-all-costs defense system.
Innate immunity is the non-specific immune system, which we can think of as our first line of defense. It includes our fortress walls, moats, and garrison soldiers. These are the barriers and forces that keep invaders out. It is non-specific in the sense that it will work hard to keep out anything that looks foreign, regardless of type. It does not concern itself with whether it has seen the invader before or not – it is a keep-out-at-all-costs defense system.
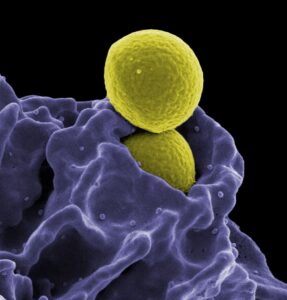
First, we must discuss the walls which are things like skin, which acts as a primary barrier to microorganisms. Along with its impenetrable membrane, it has an acidic oil on its surface which renders it uninhabitable for many bacterial species. Mucous membranes in the nasal passages, mouth, and other orifices also act as a primary barrier to pathogens seeking entry. The acidic environment of the stomach makes it unsuitable for many bacterial and viral species.
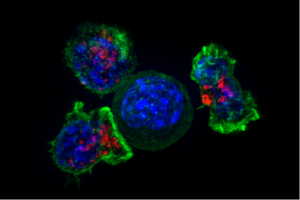
If an invader makes it through the primary barriers, gaining entry into our blood circulation, respiratory, or other organ tissue, then our garrison foot soldiers come to the defense. These cells – known as phagocytes (neutrophils, macrophages, and natural killer (NK) cells) – essentially destroy invading organisms by swallowing them up (phagocytosis) or releasing chemicals, which disrupt cellular structural elements leaving the microorganism susceptible to bursting. Phagocytes can also induce inflammation and release chemicals that send signals to recruit another class of immune cells called lymphocytes to the site of infection.
Adaptive Response Immunity
Some invaders will find entry into the kingdom. The mechanisms evolved to evade the initial onslaught may include the secretion of bacterial toxins to impair protective functions of host barriers (like ciliary clearance function [hairlike sweeping] of the respiratory tract), biofilm formation, and evasion of immune recognition, among others. Regardless of the means used to gain entry, once in, the invaders can cause maximal damage. They will initially float around the body’s extracellular fluids like the blood, lymphatic, cerebrospinal (CSF), and pleural fluid, as well as in body cavities lined with serous (moisture-exuding) membranes.
Humoral Immune Response
 Enter the humoral immune response: secreted antibodies, opsonins, and the complement system (which complements antibodies), surveilling the body fluids (humors) on a seek-and-destroy mission. When these reconnaissance satellites encounter a pathogen, they may directly kill it (complement system) as might a missile-wielding drone, coat it for recognition (opsonization) by destructive soldiers (phagocytes), or interfere (sabotage) with the chemical interactions required for the pathogen to infect or bind to other cells (antibodies).
Enter the humoral immune response: secreted antibodies, opsonins, and the complement system (which complements antibodies), surveilling the body fluids (humors) on a seek-and-destroy mission. When these reconnaissance satellites encounter a pathogen, they may directly kill it (complement system) as might a missile-wielding drone, coat it for recognition (opsonization) by destructive soldiers (phagocytes), or interfere (sabotage) with the chemical interactions required for the pathogen to infect or bind to other cells (antibodies).
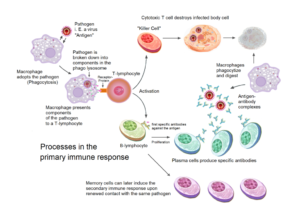
The special forces are the elite soldiers on the battlefield, and for the human immune system, these are the lymphocytes of the adaptive or specific immune response. The B lymphocytes are responsible for the humoral immune reaction. They recognize foreign antigens – molecular markers that elicit an immune response – and respond by creating antibodies specific to that marker. As a result, they become the progenitor of specific B cells which will forever recognize one specific invader – a bacteria or virus, let’s say. They differentiate into memory and plasma B cells, which are like the intelligence and munitions departments of the armed forces.
Memory B cells are long-lasting lymphocytes (some lasting decades), which present the original recognition receptor of the parent for the specific pathogen and its antigen on their surface. They are one of several antigen-presenting cells (APC), along with macrophages and dendritic cells (DC). Their primary role is to act as long-term recognition of a pathogen it has seen before, and so these cells are responsible for what we call the secondary immune response. It is what gives us long-term immunity to previous invaders.
Plasma B cells, or effector B cells, are essentially antibody production plants. They produce large quantities of long-lived antibodies specific to the pathogenic antigen of its parent cell. The antibodies are released into the fluid system to circulate throughout the body. They act as surveillance reconnaissance drones keeping on the lookout for a future invasion by the original intruder.
Cell-mediated Immune Response
So, while B cells of the humoral system produce antibodies, which in turn circulate throughout the body in search of previously encountered antigens, they are only effective against free-floating pathogens. In other words, only pathogens moving about freely in the body’s fluids are at risk from circulating antibodies. But what happens when an invader makes it inside a cell, infecting it? If antibodies are helpless against these infiltrators, then is that the end of the fight? The answer is: “Absolutely not” – this is where cell-mediated immunity comes in.
The big guns of the cell-mediated immune response are T lymphocytes (cells). Other soldiers like macrophages and NK-cells also contribute to these reactions, but cytotoxic T cells are the assassins of the immune system while helper T cells the secret police. Cell-mediated immunity is the destruction of cells that have been infiltrated. This could happen from a bacteria or virus, but it can also be a cancer cell. Any cell that needs to be eliminated will be paid a visit by one of these soldiers.
In the case of the cytotoxic T cell, the visit is paid direct. These T cells directly kill the infected or cancerous cells by poking holes into their membranes and inserting enzymes, like grenades or other IEDs, which ultimately destroy the infected cell. Like assassins, cytotoxic T cells go in, create a vulnerability, and then exploit it.
Helper T cells, on the other hand, act like the police by surveilling the body. When they encounter foreign antigens, they also act in a specific manner, like the B lymphocytes, specific to only one antigen. When activated, helper T cells differentiate into memory T cells – which are long-lasting, providing long-term immunity – and effector cells. Effector T cells are the alarm system, which sends out signals to draw in even more soldiers to the area. They also play a role in activating B cells to secrete antibodies and proliferate into memory B cells.
Inflammation, Hypersensitivity, and Autoimmunity
A healthy, robust immune system is paramount for keeping our bodies free from invaders. However, it can also be too robust. Three immune responses that can go haywire and lead to destruction and even death are inflammation, hypersensitivity, and autoimmunity.
Inflammation is a normal, healthy, and abundant immune response to injury, infection, and tissue damage; it is the engagement of the military on the battlefield. It is characterized by heat, redness, swelling, and pain at the site of injury or infection. Inflammation serves to eliminate pathogens, clear debris, and initiate tissue repair, and it recruits soldiers from both the innate and adaptive immune responses (like neutrophils and macrophages, as well as B and T lymphocytes).
A fundamental part of the inflammatory response is cytokine release, whereby signaling molecules act as messengers to initiate, amplify, and regulate the inflammatory process. It contributes to the body’s defense against infection and injury. Dysregulation of cytokine signaling can lead to chronic inflammation and contribute to the pathogenesis of various inflammatory diseases.
Hypersensitivity refers to an exaggerated or inappropriate immune response to harmless substances, known as allergens. There are four types of hypersensitivity reactions (Type I to Type IV), each involving different mechanisms and immune components. An example of hypersensitivity is allergic rhinitis (hay fever), where exposure to pollen triggers an exaggerated immune response, leading to symptoms such as sneezing, itching, and nasal congestion.

Systemic lupus erythematosus (SLE), is an autoimmune disease in which the immune system attacks its own tissues, causing widespread inflammation and tissue damage in the affected organs
Autoimmunity occurs when the immune system mistakenly targets and attacks healthy tissues and cells, leading to tissue damage and dysfunction. Autoimmune diseases can affect various organs and systems, and they are characterized by chronic inflammation and immune-mediated damage. An example of autoimmunity is rheumatoid arthritis, where the immune system attacks the joints, causing inflammation, pain, and joint damage over time.
Each process can and does have significant implications for health and disease. The cytokine storm was a hallmark of severe COVID-19 infection and has been recognized as a major cause of mortality among COVID-19 patients. Hypersensitivity may be another important mechanism involved in severe cases of COVID-19.
Epilogue
As you can see, the complexity of the human immune system is vast, and its potential to adapt to specific invaders…infinite. That makes the immune system a veritable guarantor of survival and a generator of evolution for the human species. What I have given you here is a sound overview of immunity – its soldiers, its systems, and its processes. As I have said above, I will refer back to this article often regarding other topics on immunology and health. I have attempted to organize the information and make it easily scannable to gather information quickly, and I have provided links to further reading and study. The next question I want to ask is: what can be done to enhance the immune system to increase health and wellness? Stay tuned.