I have told you all about diet and how I believe food sensitivities are responsible for the widespread prevalence of gastrointestinal (GI) disorders in the western world today. I have explained that everything from hiccups to gastroesophageal reflux disease (GERD) to irritable bowel syndrome (IBS) is the body’s response (either early or late) to physiological insult from food which acts as a poison to that body. A recent study outlines how, at least, one GI condition progresses along this path.
I have told you all about diet and how I believe food sensitivities are responsible for the widespread prevalence of gastrointestinal (GI) disorders in the western world today. I have explained that everything from hiccups to gastroesophageal reflux disease (GERD) to irritable bowel syndrome (IBS) is the body’s response (either early or late) to physiological insult from food which acts as a poison to that body. A recent study outlines how, at least, one GI condition progresses along this path.
Researchers from the University of Pittsburgh found that a high-sugar diet worsened inflammatory bowel disease (IBD) symptoms in a mouse model. Mice were fed either a standard or high-sugar diet and then treated with a chemical to mimic IBD colon damage after they were fed one of the two diets. All mice fed a high-sugar diet died within nine days of the 14-day experiment. All the mice fed a standard diet survived for all 14 days.
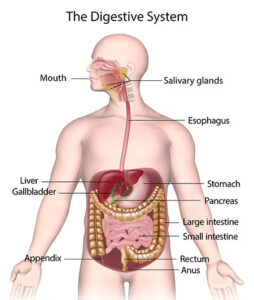 IBD is a chronic condition that affects the digestive system. It’s a term used to describe a group of disorders characterized by chronic inflammation in the gastrointestinal tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. Current medical science is uncertain of the exact cause of IBD, but believes it to be the result of an abnormal immune response in genetically susceptible individuals, triggered by environmental factors. Sound familiar? I told you in this article that when medical science does not know all the details around a pathology, the standard go-to is “genetic predisposition.” All this means is “we don’t know,” and since everything biological is foundationally genetic anyway, that explanation means very little.
IBD is a chronic condition that affects the digestive system. It’s a term used to describe a group of disorders characterized by chronic inflammation in the gastrointestinal tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. Current medical science is uncertain of the exact cause of IBD, but believes it to be the result of an abnormal immune response in genetically susceptible individuals, triggered by environmental factors. Sound familiar? I told you in this article that when medical science does not know all the details around a pathology, the standard go-to is “genetic predisposition.” All this means is “we don’t know,” and since everything biological is foundationally genetic anyway, that explanation means very little.
But according to what modern medicine does know: In IBD, the immune system mistakenly attacks the lining of the digestive tract, leading to inflammation and damage. This inflammation can occur anywhere along the digestive tract, from mouth to anus, with the severity and location of inflammation varying depending on the type of IBD and the individual. Common symptoms of IBD include abdominal pain, diarrhea (sometimes with blood), rectal bleeding, weight loss, fatigue, and reduced appetite.
Living with IBD often involves periods of active disease (flare-ups) and periods of remission. Medical science classifies IBD flare-ups as unpredictable, and as such, IBD can significantly impact a person’s quality of life, through physical discomfort, emotional distress, and limitations in daily activities. The medical approach to managing IBD typically involves medication and/or surgery. As you can see, the article I wrote on the pathophysiology of food sensitivities outlines this exact scenario associated with IBD.
So for this study, researchers examined the colons of the mice who had died following the high-sugar diet. What they found was that the lining of the large intestine was inhibited in its healing and regeneration as signified by diminished expression of cells (intestinal stem cells [ISCs]) needed to maintain barrier integrity of the colon walls, especially after inflammatory damage.
As you can imagine, these stem cells are very important in regenerating damaged epithelium and must divide even faster to replace dead and damaged cells. What we found was that high sugar concentrations directly affected the ability of stem cells in the intestine to regenerate in response to damage. Under high sugar conditions, when they need to increase their function, intestinal stem cells were unable to do so.
– Tim Hand, PhD, senior study author
 The study authors, naturally, advise people with IBD to avoid high-sugar intake, especially soda and candy. I will take it a step further and say, try to avoid sugar completely, except for very rare occasions, IBD or not. As I pointed out in my article from 2013, everybody walking the planet has foods to which they are sensitive. These foods act as toxins to that person. In over two decades of observation, I have found that refined sugar is poisonous, and I mean with extremely rare exception, to practically every person. This study on mice being administered high-sugar diets simply confirms what I have been sharing with you over the last ten years: and it gives a peek into the pathophysiology of the process. If you are interested in the biochemistry involved in the study, you can read it here: Excess Dietary Sugar Alters Colonocyte Metabolism and Impairs the Proliferative Response to Damage
The study authors, naturally, advise people with IBD to avoid high-sugar intake, especially soda and candy. I will take it a step further and say, try to avoid sugar completely, except for very rare occasions, IBD or not. As I pointed out in my article from 2013, everybody walking the planet has foods to which they are sensitive. These foods act as toxins to that person. In over two decades of observation, I have found that refined sugar is poisonous, and I mean with extremely rare exception, to practically every person. This study on mice being administered high-sugar diets simply confirms what I have been sharing with you over the last ten years: and it gives a peek into the pathophysiology of the process. If you are interested in the biochemistry involved in the study, you can read it here: Excess Dietary Sugar Alters Colonocyte Metabolism and Impairs the Proliferative Response to Damage
This study is particularly relevant considering the average American consumes somewhere between 17-34 teaspoons per day, which is more than six times the recommended intake by the American Heart Association. This averages more than 100 pounds of sugars per person each year. Almost all processed foods in the supermarket contain extra sugar and this includes and many “low fat” products. Sodas, themselves, contain 10 teaspoons of sugar per can. High Fructose corn syrup (HFCS) has replaced sucrose (sugar) in many food products. HFCS is only sold for processed foods; yet, it provides about 8% of the total calories in the average American diet.
 Food sensitivities are a reality for all people. Which foods are poisons for which people vary by type. Finding out which foods you should avoid is paramount to preserving your gastrointestinal health. If you find yourself in Los Angeles or Palm Springs (the Coachella Valley), then I am available for consultations. We can find your specific body type, and thus the foods which are toxic to you, and also those which are tonic – or beneficial – to your digestive disposition. What can you do on your own in the meantime? Pay attention to the moments you do not feel well in any part of the digestive system – from mouth to anus – and record the foods you had just before your symptoms arose. It will take patience and perseverance to find the offenders, but if you remove those suspicious foods from your diet, while also removing symptoms, then you are those many steps closer to figuring things out. If you have IBD of any form, I assure you that something in your diet is causing that situation. Very likely sugar is a major contributing factor, but sugar may not be the only problem – so you will have to look. However, this study shows clearly how at least one substance (refined sugar) acts as a toxin to diminish the healing capacity of the colon and its ability to regenerate as needed. Like I said in 2013, from source of irritation, to symptoms, to chronic condition, to frank disease over time. I’ve been watching it unfold – and helping people with real solutions – for over twenty years.
Food sensitivities are a reality for all people. Which foods are poisons for which people vary by type. Finding out which foods you should avoid is paramount to preserving your gastrointestinal health. If you find yourself in Los Angeles or Palm Springs (the Coachella Valley), then I am available for consultations. We can find your specific body type, and thus the foods which are toxic to you, and also those which are tonic – or beneficial – to your digestive disposition. What can you do on your own in the meantime? Pay attention to the moments you do not feel well in any part of the digestive system – from mouth to anus – and record the foods you had just before your symptoms arose. It will take patience and perseverance to find the offenders, but if you remove those suspicious foods from your diet, while also removing symptoms, then you are those many steps closer to figuring things out. If you have IBD of any form, I assure you that something in your diet is causing that situation. Very likely sugar is a major contributing factor, but sugar may not be the only problem – so you will have to look. However, this study shows clearly how at least one substance (refined sugar) acts as a toxin to diminish the healing capacity of the colon and its ability to regenerate as needed. Like I said in 2013, from source of irritation, to symptoms, to chronic condition, to frank disease over time. I’ve been watching it unfold – and helping people with real solutions – for over twenty years.