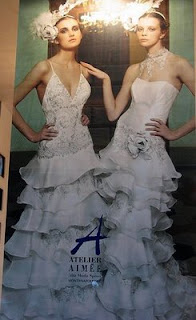
Bravo to Vogue magazine…bravo. I have been saying for over a decade that if we want to make a dent in the perpetuation of eating disorders, it has to start with the images we choose to look at regularly, the ones we choose to deem “beautiful.” Well, Vogue mag is doing its part by banning the images of “too-skinny” models. Duh! And Bravo.
Not only is the mega-fashion mag doing away with too-skinny, but too-young is being flung, too. The 19 Vogue magazine editors around the world made a pact to project healthy, not ultra-thin. They agreed to “not knowingly work with models under the age of 16 or who appear to have an eating disorder,” and said they will ask casting directors to check IDs at photo shoots and fashion shows and for ad campaigns.
Most editions of Vogue made it common practice to hire girls under 16–a sure road to a future eating disorder. I mean think about it–which model isn’t going to psych-out when comparing herself to her immature, underdeveloped 14-year-old self?
 “I want my prepubescent figure back…” Duh!
“I want my prepubescent figure back…” Duh!
But, of course, not just models: Every young adult, teen, and heck…many women of all ages look to fashion magazines like Vogue for ideas on the latest looks, and these unfortunately…and probably subconsciously…include body types. I cannot tell you how many women I have heard say, “But clothes just hang better when you’re thin.”
My retort, “No…you just have set the convoluted images in fashion and celebrity magazines as your relative point…the standard,” if you will.
 Seems that Vogue, however, is just following a healthy trend. The Council of Fashion Designers of America adopted a voluntary initiative in 2007, which emphasizes age minimums and healthy working environments during New York Fashion Week, and London Fashion Week designers sign a contract with the British Fashion Council to use models who are at least 16.
Seems that Vogue, however, is just following a healthy trend. The Council of Fashion Designers of America adopted a voluntary initiative in 2007, which emphasizes age minimums and healthy working environments during New York Fashion Week, and London Fashion Week designers sign a contract with the British Fashion Council to use models who are at least 16.
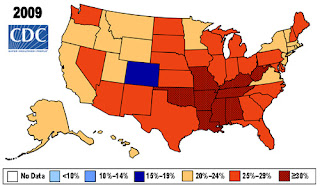
 The primary fashion organizations in Italy and Spain banned catwalk models who fall below a certain body mass index (BMI) level, and earlier this year, Israel’s government passed an anti-skinny-model law. This all on the heels of the deaths of two young models in 2006-2007 following complications from eating disorders.
The primary fashion organizations in Italy and Spain banned catwalk models who fall below a certain body mass index (BMI) level, and earlier this year, Israel’s government passed an anti-skinny-model law. This all on the heels of the deaths of two young models in 2006-2007 following complications from eating disorders.





 25 kg m−2 before pregnancy and after 16-year follow-up) was the strongest single predictor.
25 kg m−2 before pregnancy and after 16-year follow-up) was the strongest single predictor.