This Saturday, I awoke to my teenage daughter stumbling through the hallway. I could hear her from my bed and knowing the sound of her footsteps, I called out, “You okay, honey?” She was dizzy she said, and her eyes were blurry. I jumped out of bed, ran to her, and helped her into the kitchen where I sat her down. We took her temperature – she was burning up. I could feel her back was sweaty and her cheeks were rosy red; I asked about her symptoms. She said she was hot and had a cough, and that was it. The momentary dizziness was just that, momentary; and her eyes were clearing. It was evident that she was fighting an infection.
This Saturday, I awoke to my teenage daughter stumbling through the hallway. I could hear her from my bed and knowing the sound of her footsteps, I called out, “You okay, honey?” She was dizzy she said, and her eyes were blurry. I jumped out of bed, ran to her, and helped her into the kitchen where I sat her down. We took her temperature – she was burning up. I could feel her back was sweaty and her cheeks were rosy red; I asked about her symptoms. She said she was hot and had a cough, and that was it. The momentary dizziness was just that, momentary; and her eyes were clearing. It was evident that she was fighting an infection.
My daughter had been under the weather for a couple of weeks. She was sick for several days two weeks prior then got better. There were four good days and then last Friday she felt ill again. She had congestion with a runny nose for most of the week, and the cough, that incessant cough. When I came home last night, she looked weathered. She had just woken up but clearly felt ill. I suggested she stay home from her theater rehearsal – her school’s rendition of Mama Mia – in which she has the role of the mother; essentially lots of singing. I didn’t want her to strain her voice, nor did I want her to expose the other students. She insisted that the show MUST go on, so I didn’t press. But her body, in its infinite wisdom, said otherwise.
Her immune system kicked into full gear, that was obvious to me. But I am certain she had put it under extreme pressure, as so many achieving young students do, so they may become susceptible to bouts of infection and illness due to what we often refer to as run-down bodies. What we mean by run-down is fatigued – often physically and mentally – sometimes malnourished, and under moderate to extreme stress. As a senior, my daughter had all these, navigating college applications (she got into four UCs, including Berkeley and UCLA; she has chosen UCLA), her AP classes (she still must pass), a boyfriend and social life, and of course, the school musical. She was run-down and tired.
In this article, I will discuss factors that diminish or enhance immune function. I will explain why you are more prone to getting ill when run down, and how to strengthen your constitution to better handle those times when you push yourself to the extreme to accomplish your goals. This article is especially useful for high school and college students to understand how they could be beating themselves down by making certain habits and lifestyle choices. It will also investigate how to mitigate this from happening, and what people can do to recover quickly and completely if they do end up running themselves into the ground.
Faulty Behaviors Suppress Immune Function
![]()
![]()
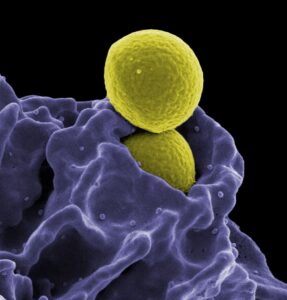
![]() So why did my daughter’s immune system fail to keep out whatever had overrun her body? How did the barriers to the fort break down and the soldiers get overwhelmed? The answer lies in resources – that is, what you provide to your defense warriors in terms of energy (nutrition), alertness (rest), and morale (lack of stress). What you do, and how you live, on a day-to-day matter when it comes to immune function. The immune system needs a certain environment in which to flourish, and if that environment is compromised, a weakened immune system, and imminent invasion, are sure to follow.
So why did my daughter’s immune system fail to keep out whatever had overrun her body? How did the barriers to the fort break down and the soldiers get overwhelmed? The answer lies in resources – that is, what you provide to your defense warriors in terms of energy (nutrition), alertness (rest), and morale (lack of stress). What you do, and how you live, on a day-to-day matter when it comes to immune function. The immune system needs a certain environment in which to flourish, and if that environment is compromised, a weakened immune system, and imminent invasion, are sure to follow.
The three most common factors suppressing the immune system are poor nutrition, chronic stress, and immunosuppressive medication. In my book, The Six Keys to Optimal Health, I outline the six key areas you must attend to regularly to attain and maintain optimal wellness. Poor nutrition and immunosuppressive medication violate keys number one (enhance diet) and six (minimize toxins), while chronic stress violates the other four. I will touch on these three primary suppressive factors and then discuss the top three things you can do to optimize your immune function.
Malnutrition as an Immune Suppressant
Inadequate intake of essential nutrients can weaken the immune system, impairing its ability to function properly. As you know from my previous writing, I believe that people have genetic, metabolic, and physiological differences (we can call them digestive constitutions) that lead them to process, or fail to process, certain foods that others have no problem processing, or in fact may thrive in processing, due to their own constitutional makeup. As a result, people who regularly eat foods that are poorly digestible to them will suffer malnutrition.
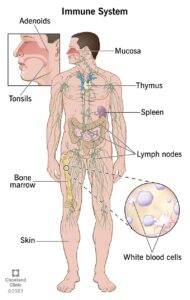
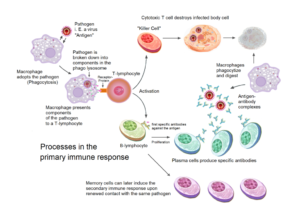
 Deficiencies in essential nutrients such as vitamins A, C, D, E, and zinc can weaken the immune system. These nutrients play critical roles in supporting various immune functions, including the production and function of immune cells, antibody production, and the regulation of inflammation. For example, vitamin C is known to enhance the function of certain immune cells like T cells and phagocytes, while vitamin D plays a role in modulating immune responses. A lack of these nutrients can impair immune function, making individuals more susceptible to infections.
Deficiencies in essential nutrients such as vitamins A, C, D, E, and zinc can weaken the immune system. These nutrients play critical roles in supporting various immune functions, including the production and function of immune cells, antibody production, and the regulation of inflammation. For example, vitamin C is known to enhance the function of certain immune cells like T cells and phagocytes, while vitamin D plays a role in modulating immune responses. A lack of these nutrients can impair immune function, making individuals more susceptible to infections.
Do not mistake malnutrition for the images you have seen of starving children in Third World countries – they are malnourished no doubt – but you can be well-fed and malnourished too. Malnourishment is the “lack of proper nutrition, caused by not having enough to eat, not eating enough of the right things, or being unable to use the food that one does eat,” according to the dictionary definition. The takeaway here is that if you are not eating enough food (willful caloric restriction), not getting the proper nutrients (poor dietary habits; junk food and whatnot) or eating foods that are wrong for your body type (constitution), you will suffer malnutrition.
Poor nutrition –> Depressed immune system –> More and longer lasting infections/illness
Chronic Stress = Immune Depressed
 Stress is defined as a state of physical, mental, or emotional tension due to challenging circumstances. When extreme or long-standing (chronic), stress can diminish health. While stress can be physical, like from extreme or excessive work, it can also tax the mental and emotional states, whether the physical is involved or not. Physical activity (or lack thereof), sleep, pain (acute or chronic), and mental health all play roles in stress. Often, several or all of these areas are taxed in the chronically stressed person.
Stress is defined as a state of physical, mental, or emotional tension due to challenging circumstances. When extreme or long-standing (chronic), stress can diminish health. While stress can be physical, like from extreme or excessive work, it can also tax the mental and emotional states, whether the physical is involved or not. Physical activity (or lack thereof), sleep, pain (acute or chronic), and mental health all play roles in stress. Often, several or all of these areas are taxed in the chronically stressed person.
Cortisol and catecholamines, such as adrenaline (epinephrine) and noradrenaline (norepinephrine), are stress hormones produced by the adrenal glands. These hormones play crucial roles in the body’s fight-or-flight response, which helps individuals respond to acute stressors or threats. However, chronic or prolonged exposure to stress can dysregulate the production and activity of cortisol and catecholamines, leading to suppression of the immune system through several mechanisms:
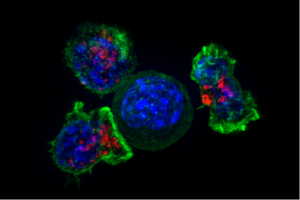
- Suppression of Immune Cell Function: Cortisol and catecholamines can inhibit the function of various immune cells, including T cells, B cells, and natural killer (NK) cells. These hormones can directly interfere with the signaling pathways involved in immune cell activation and proliferation, impairing their ability to mount effective immune responses against pathogens.
- Decreased Production of Inflammatory Mediators: Cortisol is a potent anti-inflammatory hormone that can suppress inflammation. By dampening the inflammatory response, cortisol helps mitigate tissue damage and inflammation associated with stress. However, prolonged suppression of inflammatory mediators can also weaken the body’s ability to combat infections and other threats.
- Alteration of Immune Cell Trafficking: Cortisol and catecholamines influence the movement and transportation of immune cells throughout the body. For example, these hormones can promote the redistribution of immune cells from the skin and mucosal surfaces to lymphoid organs like the thymus and spleen. While this helps limit tissue damage during acute stress, it also compromises immune surveillance and responsiveness in peripheral tissues, increasing the risk of infections.
- Shift in Immune Response: Chronic stress and elevated levels of cortisol and catecholamines can bias the immune system towards a Th2-type immune response (humoral response), and suppression of Th1-type responses (cellular immune response). This shift in immune balance, a hallmark of the allergy response, can impair the body’s ability to mount an effective immune response against intracellular pathogens, such as viruses and certain bacteria.
From an evolutionary perspective, the suppression of immediate immune function from a heightened stress response serves multiple adaptive functions. First, it conserves energy by redirecting resources towards essential bodily processes required for immediate survival, like increasing heart rate and blood flow to muscles, while suppressing non-essential functions such as digestion and immune responses. Additionally, it helps prevent excessive inflammation and tissue damage that could arise from immune cells, thus preserving tissue integrity. Finally, it may safeguard against autoimmune reactions by temporarily reducing immune cell activation and proliferation. However, prolonged stress can have adverse effects on immune function and overall health, underscoring the importance of managing stress levels for optimal well-being.
 Lack of sleep can also make us more susceptible to getting sick, while good sleep is crucial for recovering from illness. The brain and immune system talk to each other constantly, meaning changes in sleep can affect our immune system and vice versa. Research on animals deprived of sleep has revealed a gradual decline in energy balance and overall health, eventually leading to a fatal bloodstream infection even without a clear source of infection.
Lack of sleep can also make us more susceptible to getting sick, while good sleep is crucial for recovering from illness. The brain and immune system talk to each other constantly, meaning changes in sleep can affect our immune system and vice versa. Research on animals deprived of sleep has revealed a gradual decline in energy balance and overall health, eventually leading to a fatal bloodstream infection even without a clear source of infection.
An increase in disease susceptibility was also observed in sleep-deprived humans. For instance, less efficient sleep and shorter sleep duration in the weeks leading up to contact with a rhinovirus were linked to reduced resistance to the common cold. One study has shown that inadequate sleep was associated with ~50% decline in the body’s ability to respond effectively to vaccines. Both limiting sleep and total sleep deprivation have been linked to weakened immune function, making individuals more prone to infections and susceptible to chronic diseases.
Finally, stress has been demonstrated to elevate the likelihood of developing autoimmune diseases. Remember autoimmunity occurs when the immune system mistakenly targets and attacks healthy tissues and cells within the body, leading to tissue damage and dysfunction. Additionally, individuals with autoimmune conditions have trouble regulating their immune responses following exposure to stressors.
Medication can Suppress Immune Function
Certain medications, such as corticosteroids, immunosuppressants used in organ transplantation, and chemotherapy drugs, are designed to suppress immune responses. While these medications are essential for managing conditions like autoimmune diseases and preventing organ rejection, they can also weaken the immune system and increase the risk of infections.
Corticosteroids (steroids), for example, work by mimicking the effects of cortisol. They inhibit the activity of immune cells and reduce the production of inflammatory mediators, thereby suppressing immune responses. Due to their use as a super-inflammation reducer, these are some of the most commonly asked-about medications in my chiropractic practice.
While steroids can be highly effective in alleviating symptoms and controlling inflammation, they inhibit the production and activity of inflammatory mediators and immune cells. Steroids dampen the body’s ability to mount an immune response, making individuals more susceptible to infection. Additionally, steroids can interfere with the function of white blood cells, such as lymphocytes and macrophages. Therefore, the use of steroids requires careful consideration and monitoring to minimize the risk of immune suppression and associated complications. I tell my patients: Use steroids sparingly.
Healthy Lifestyle Behaviors Enhance Immune Function
To the same degree that faulty lifestyle behaviors can suppress immune function, so too can healthy behaviors enhance it. The three most important and wide-reaching activities you can adopt for optimal immunity are maintaining a healthy diet, exercising regularly, and getting sufficient sleep. High school and college students need to maintain these behaviors before and during their semesters, as the rigors of studying can run the bodies down. Having a conditioned and heightened immune system will get them through those late nights and busy schedules, protecting them even when their peers are falling ill around them.
Healthy Diet
The most important thing you can do for your dietary health is to eat according to your body constitution (see above). Depending on where you are in the world, I might be able to help you with a referral. If you live in Los Angeles or the Coachella Valley, I can help you directly with testing and dietary/nutritional analysis. Outside of that, you can practice some basic dietary/nutritional habits:
First is to make sure you eat whole, natural foods. Whether you abide by an animal-based diet or a plant-based one, making sure you have real food is crucial. In a nutshell, this means fresh, store-bought food, prepared at home – not canned or packaged, not premade, and not fast food. Eating at a regular rhythm is also essential for optimal dietary health. In other words, food type (believe it or not, less variety is better than more) proportion, and consistent feeding time are vital to optimizing nutrition.
 Nutrients that enhance immune function include vitamins (e.g., vitamin C, vitamin D, vitamin E), minerals (e.g., zinc, selenium), fatty acids (omega 3s), and phytochemicals (e.g., flavonoids, carotenoids), which play crucial roles in various aspects of immunity, such as antibody production, cellular immunity, and inflammation regulation.
Nutrients that enhance immune function include vitamins (e.g., vitamin C, vitamin D, vitamin E), minerals (e.g., zinc, selenium), fatty acids (omega 3s), and phytochemicals (e.g., flavonoids, carotenoids), which play crucial roles in various aspects of immunity, such as antibody production, cellular immunity, and inflammation regulation.
An “activated” immune system increases the body’s energy needs, especially during infections when basal energy expenditure rises, as seen in fever. Therefore, optimal nutrition for ideal immune function would support immune cell activities, enabling them to mount effective responses against pathogens while swiftly resolving the response when needed and preventing chronic inflammation.
Regular Exercise
 Next, you must get regular movement in the form of exercise. Regular physical activity boosts immune function by promoting circulation and reducing inflammation. As the blood flows, white blood cells (leukocytes) spread throughout the body, as do antibodies and immune factors. These cells become more readily available at new penetration and infection sites.
Next, you must get regular movement in the form of exercise. Regular physical activity boosts immune function by promoting circulation and reducing inflammation. As the blood flows, white blood cells (leukocytes) spread throughout the body, as do antibodies and immune factors. These cells become more readily available at new penetration and infection sites.
Regular exercise also stimulates the production of immune cells, like neutrophils, macrophages, and natural killer (NK) cells—soldiers that play key roles in the innate immune response. These cells detect and destroy pathogens, infected cells, and cancer cells. Studies show that single bouts of moderate-intensity exercise are “immuno-enhancing” and have been used to effectively increase vaccine responses in “at-risk” patients.
Moreover, exercise can help reduce chronic low-grade inflammation associated with many chronic diseases. By modulating inflammatory cytokines and promoting anti-inflammatory processes, exercise helps maintain a balanced immune response and reduce the risk of inflammatory-related conditions.
Finally, exercise is known to reduce stress, a major player in immune suppression. But a word of caution: prolonged intensive exercise can do the opposite and act as a stress on the body, thereby diminishing immune function and increasing susceptibility to illness. Extended periods of exercise can hinder the function of T cells, NK cells, and neutrophils, disrupt the balance of Type I and Type II cytokines, and weaken the body’s immune responses to initial and repeated exposure to antigens. Elite athletes frequently report symptoms associated with upper respiratory tract infections (URTI) when engaging in intense training and competition, which could stem from changes in mucosal immunity, notably decreases in secretory immunoglobulin A levels.
Adequate Sleep
Last but not least, is the absolute necessity of getting regular, sufficient sleep. Doing so is crucial for maintaining a healthy immune system, as sleep helps regulate immune function and promotes the production of immune cells. During sleep, the body undergoes various immune processes, including the production and release of cytokines (proteins that regulate immune responses) and the activation of immune cells. Chronic sleep deprivation can disrupt these processes.
![]()
 During sleep, the body produces and releases T cells, B cells, and natural killer (NK) cells. Studies show that sleep deprivation can lead to a decrease in the number and activity of these immune cells. Adequate sleep helps ensure optimal immune cell production and function, strengthening the body’s defense against pathogens.
During sleep, the body produces and releases T cells, B cells, and natural killer (NK) cells. Studies show that sleep deprivation can lead to a decrease in the number and activity of these immune cells. Adequate sleep helps ensure optimal immune cell production and function, strengthening the body’s defense against pathogens.
Sleep is also vital in modulating inflammatory responses in the body. Chronic sleep deprivation is associated with increased levels of pro-inflammatory cytokines, which can contribute to chronic inflammation and various health problems. In contrast, sufficient sleep promotes the release of anti-inflammatory cytokines, helping to maintain a balanced immune response and reduce the risk of inflammatory-related diseases.
Finally, sleep is essential for the formation and maintenance of immune memory (adaptive immune response), which allows the body to mount a faster and more robust immune response. Individuals who get adequate sleep after receiving a vaccine develop stronger and longer-lasting immune responses compared to those who are sleep-deprived. This highlights the importance of sleep in mounting an effective consolidation of immune memory.
Why Highschool and College Students are Prone to Falling Ill
 When we think of the life of an ambitious student, we acknowledge that they have a rigorous schedule that often includes academic pressures, work responsibilities, and maintaining an active social life. While not all students have to attend to these obligations equally – some do not work, others have low social interest – they tend to distribute their time to their obligations similarly. The intense attention they place on one or all three (sometimes even more) areas, can lead them to run down physically, mentally, and emotionally.
When we think of the life of an ambitious student, we acknowledge that they have a rigorous schedule that often includes academic pressures, work responsibilities, and maintaining an active social life. While not all students have to attend to these obligations equally – some do not work, others have low social interest – they tend to distribute their time to their obligations similarly. The intense attention they place on one or all three (sometimes even more) areas, can lead them to run down physically, mentally, and emotionally.
Lack of adequate or restful sleep, particularly when extended over the length of weeks, can severely depress the immune system. This is likely the number one cause of students getting sick, and for holding onto their illness for longer than usual times. It highlights the importance of students learning and applying good and regular sleep habits before they enter college. In other words, high school is probably the time students must learn the importance of sleep. Caretakers (parents) should remind and encourage students to get as much sleep as they can. If the student brings poor sleep habits into college, their performance and health will surely suffer.
Sleep deprivation also renders the student more susceptible to stress. Add to that the demands of school work, competition for grades and graduate positions, work stresses, relationship breakups, and potential family problems, and the environment is ripe for a depressed immune system. Nobody can mitigate all sources of stress, but one can strengthen the body and mind to be better able to handle the stresses as they come.
First is physical health, so diet and exercise are paramount in building up the internal environment. Good wholesome food prepared at home is the most important thing you can do in this regard. Then, regular movement done multiple times per week, enough to make you sweat, but without over-training (which can depress the immune system), is the next best thing you can do to strengthen your inner environment. If you have injuries – from sports, accidents, or anything else – have a doctor who works naturally with the body itself adress them (chiropractor, acupuncturist, or massage therapist), and try to avoid taking medications, especially steroids for inflammation control when you can use ice instead. Doing so will lower your risk of immunosuppression which comes as a side effect of using corticosteroids.
Next is mental health, and again, there is no cookie-cutter system to mitigate the many stresses students encounter from semester to semester. But prioritizing is a solid action students can take to maximize their potential for academic survival and success. It may seem that school matters should come first, but in reality, it is your health that should take top priority. Of course, students have a goal in mind, and their future will seem to depend on prioritizing academic matters. However, without a strong body and mind, academics will take a backseat anyway.
Getting sick costs energy and time, so minding their wellness is paramount to your accomplishments. Then each individual will have to determine the next priority, whether that be work, social life, clubs, and so on. There is no right or wrong, but you must keep in mind that the day only has 24 hours, and you would be wise not to steal from your sleep time to accommodate other, lesser priorities (a common miscalculation by students).
If you do get sick, the order of importance is rest, nutrition, medical help if you need it (could be priority number one if a life-threatening illness), and then strengthening through exercise. And then refrain from jumping into the patterns of neglect and poor choice that got you ill in the first place.
My daughter, it turns out, had the flu. She had no body aches so that threw me. I did take her to the Children’s Hospital in Hollywood, where she received the diagnosis…and orders to stay home, rest, and drink lots of fluids. That’s what we did. She really ran herself down. With school, her play, and college applications/decisions, she burned the candle at both ends (not to mention her attention to social life, to boot). She had to learn through experience that health comes first, then school, then everything else.
Students, and all people, need to be smart and take care of their bodies and minds. Depressing health through poor lifestyle behaviors is counterproductive. While each experience eventually teaches you what to do and not do, heed my advice early on to maximize the shots you have today. School life is taxing, and so is work-life, social life, and every other life of an adult. Do the right things and have the strength (and fortified environment, with soldiers at the helm) to protect you when times get tough. In so doing, you stand the greatest chance of success and maximizing your life experience.